Bunions are a very common foot condition that often start subtly but can progress into a serious, painful deformity if not addressed early. For many people, the appearance of a bunion may seem like just a cosmetic concern at first—a small bump near the base of the big toe that makes wearing certain shoes uncomfortable. But as the deformity worsens, pain, swelling, joint stiffness, and mobility issues often follow. If you’re one of the many people struggling with bunions, you might wonder if surgery is the best option to correct the problem—or whether there are other ways to manage the condition.
The decision to pursue bunion surgery is a personal one and depends on many factors, including your level of pain, foot function, and quality of life. In this comprehensive guide, we’ll help you better understand what bunions are, why they form, the symptoms they cause, and when surgery becomes an appropriate consideration. With the right information, you can make empowered decisions about your foot health and explore treatment options that restore comfort and mobility.
What Is a Bunion?
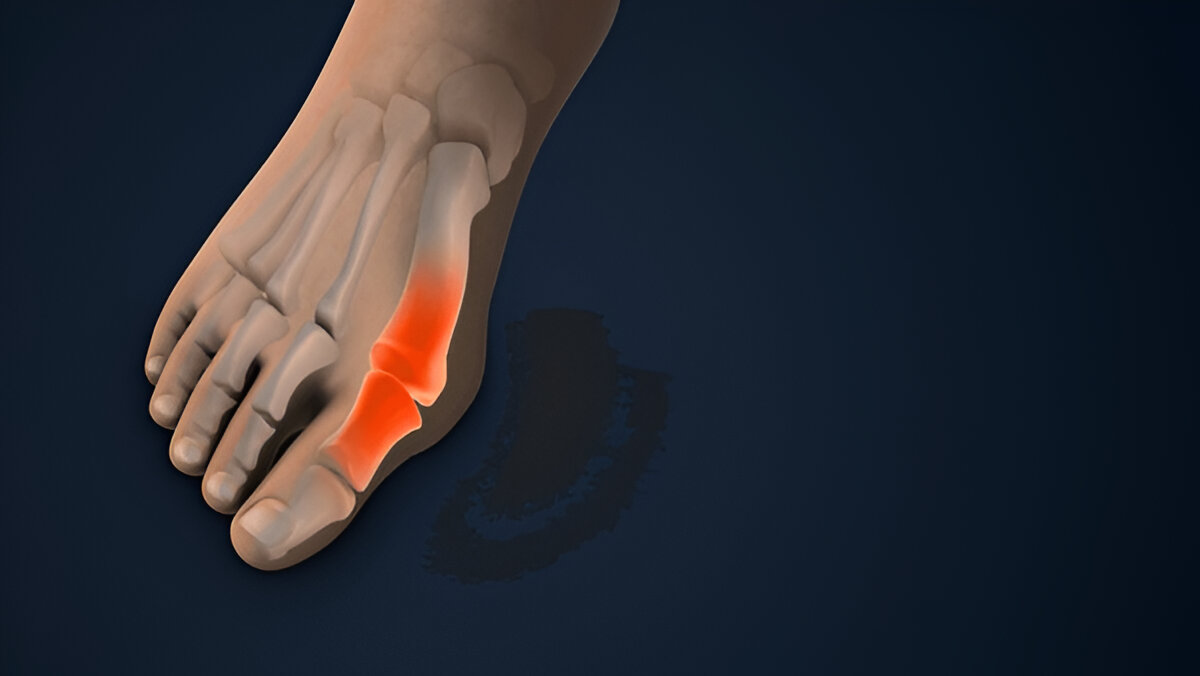
A bunion, also known as hallux valgus, is a progressive deformity of the foot in which the big toe drifts inward toward the second toe while the first metatarsal bone shifts outward. This misalignment causes the base of the big toe joint to protrude outward, forming a visible bump on the side of the foot. Over time, the joint becomes inflamed, irritated, and arthritic, which contributes to stiffness, pain, and difficulty wearing shoes.
As the deformity progresses, the biomechanics of the foot are altered. The big toe joint no longer functions efficiently during walking, which forces other parts of the foot to compensate. This can lead to additional problems such as metatarsalgia (pain in the ball of the foot), hammertoes, and calluses. Understanding that a bunion is more than just a bump—it is a structural imbalance of the foot—helps explain why treatment often involves more than cosmetic correction.
Left untreated, bunions tend to worsen with time, particularly if the person continues to wear ill-fitting shoes or has underlying foot mechanics that encourage progression. Seeking professional care early can help slow the deformity and minimize long-term damage.
Why Do Bunions Develop?
The development of bunions is typically the result of a combination of genetic, biomechanical, and lifestyle factors. One of the most significant contributors is heredity. If bunions run in your family, your chances of developing them are greatly increased. Often, it’s not the bunion itself that’s inherited but rather a certain foot type—such as flat feet, low arches, or excessive pronation—that predisposes you to the deformity.
Wearing poorly designed footwear, such as narrow-toed shoes or high heels, can exacerbate an existing tendency toward bunion formation. Shoes that force the toes into unnatural positions accelerate the misalignment of the big toe joint and place repetitive stress on the first metatarsal. In cultures where tight or heeled footwear is common, bunions are more prevalent compared to populations who regularly go barefoot or wear supportive, wide-toed shoes.
Additional risk factors include arthritis, especially inflammatory types like rheumatoid arthritis, which can destabilize foot joints. Foot injuries, ligament laxity, and neuromuscular conditions can also contribute. While not all bunions are preventable, modifying your footwear and addressing mechanical issues can help reduce their progression.
Symptoms of Bunions
Recognizing the Signs
Bunions often develop gradually, and early symptoms may be mild enough to ignore. Many patients initially notice a slight bulge or bump near the base of the big toe, which may only cause occasional discomfort when wearing snug shoes. Over time, however, symptoms tend to increase in severity.
As the bunion enlarges, you may experience chronic pain, particularly while walking or standing for long periods. Swelling, redness, and a burning sensation are common at the bunion site due to joint inflammation. The big toe’s increasing drift toward the second toe may cause friction between the toes, leading to painful corns or calluses.
In more advanced stages, limited range of motion in the big toe becomes noticeable, making it difficult to push off properly during walking. Balance may also be affected as weight distribution across the foot changes. When left unaddressed, bunions can lead to complications such as hammertoes, neuromas, and joint degeneration that severely limit mobility and quality of life.
When Should You See a Podiatrist?
The Importance of Early Evaluation
Many people delay seeking treatment for bunions because they assume the condition is merely cosmetic or “not bad enough yet” for medical attention. However, early evaluation is critical to preserving joint function and preventing further complications. Even mild bunions can benefit from conservative care that slows the deformity.
You should consult a podiatrist if your bunion causes persistent pain that interferes with walking or exercise, or if you notice that your big toe is drifting further out of alignment. If you develop corns, calluses, or other toe deformities, a podiatrist can provide preventive interventions.
Additionally, if footwear is becoming increasingly difficult to fit, or if your bunion is impacting your daily activities, a professional assessment is warranted. X-rays can determine the degree of joint misalignment and help guide treatment recommendations. Addressing bunions early may help you avoid or delay the need for surgery.
Non-Surgical Treatment Options for Bunions
Managing Pain and Preventing Progression
Not all bunions require surgery, especially if caught in their early stages. Conservative treatments focus on relieving discomfort, improving joint mobility, and slowing the bunion’s progression. While non-surgical options won’t “reverse” the deformity, they can significantly enhance quality of life and delay the need for surgical intervention.
Switching to roomier, supportive footwear is one of the simplest and most effective changes you can make. Look for shoes with wide toe boxes, cushioned soles, and good arch support. Orthotics can also help by correcting abnormal foot mechanics and redistributing pressure away from the bunion joint.
Other conservative measures include toe spacers, bunion pads, anti-inflammatory medications, and ice therapy for flare-ups. Physical therapy exercises can strengthen surrounding muscles and improve joint flexibility, helping to stabilize the big toe joint and improve gait mechanics. A personalized treatment plan from your podiatrist can make a world of difference in managing bunion-related pain.
When to Consider Bunion Surgery
Weighing the Decision for Surgical Correction
Deciding to pursue bunion surgery is often a gradual process. Many patients can manage mild to moderate bunions successfully for years through conservative care. However, when symptoms become persistent and significantly impact daily life, surgery becomes a more attractive option.
You might consider surgery if bunion pain persists despite changes in footwear and orthotics, or if joint stiffness and deformity are interfering with walking and exercise. Some patients choose surgery when they can no longer find shoes that fit comfortably or when secondary problems like hammertoes or arthritis develop.
It’s important to remember that the goal of bunion surgery is not cosmetic—it is to restore foot function, relieve pain, and correct deformity to prevent further joint damage. Consulting with an experienced foot surgeon can help you understand your options and whether surgical correction is appropriate for your specific condition.
Types of Bunion Surgery
Surgical Techniques and Expectations
There are several types of bunion surgery, and your surgeon will choose the technique that best matches your foot structure and the severity of your bunion. The most common procedure is an osteotomy, in which the metatarsal bone is cut and repositioned to correct alignment. Screws or pins may be used to stabilize the bone during healing.
For more severe deformities or when joint degeneration is present, more complex procedures such as arthrodesis (joint fusion) or Lapidus procedures (fusion of the first metatarsal) may be recommended. These surgeries not only address the bunion but also improve the overall structural balance of the foot.
Advances in minimally invasive techniques have improved recovery times and cosmetic outcomes. Recovery typically involves a period of protected weight-bearing in a surgical shoe or boot, followed by physical therapy to restore mobility and strength. A well-executed bunion surgery can dramatically improve pain relief, foot alignment, and walking function.
What to Expect After Bunion Surgery
Recovery, Healing, and Long-Term Outcomes
Recovery from bunion surgery varies depending on the procedure performed and the severity of your bunion. In most cases, patients wear a surgical boot or protective shoe for 4-6 weeks and gradually resume weight-bearing under the guidance of their surgeon. Swelling typically persists for several months, and full healing of the bone can take 3-6 months.
Physical therapy is often recommended to restore range of motion in the big toe joint and strengthen foot and ankle muscles. Many patients are able to return to normal activities within 3-4 months, though impact sports may require a longer recovery period.
Most importantly, bunion surgery offers excellent long-term outcomes when performed by an experienced surgeon and combined with appropriate rehabilitation. Patients typically experience dramatic improvements in pain relief, shoe fit, mobility, and overall foot appearance. Following your surgeon’s post-operative instructions carefully will help ensure a smooth recovery and minimize the risk of recurrence.
Garden State Foot & Ankle Group: Your Partner in Bunion Care
If you’re living with bunion pain or wondering whether surgery is the right choice for you, the team at Garden State Foot & Ankle Group is here to help. Led by board-certified foot and ankle surgeon Dr. Manooj Prasad, we offer comprehensive evaluation and both conservative and surgical treatment options for bunions.
We believe in personalized care—whether you’re managing a mild bunion conservatively or considering surgery for a more advanced deformity. Our team will take the time to understand your lifestyle, goals, and symptoms, then develop a tailored treatment plan to help you walk comfortably again. You don’t have to live with bunion pain. Relief is possible—and we can help you get there.
Take the First Step Toward Relief Today
If you’re ready to address your bunion pain, don’t wait. The earlier you seek care, the more options you’ll have for restoring foot health and preventing further damage. Contact Garden State Foot & Ankle Group today to schedule your consultation and take the first step toward lasting relief. We look forward to helping you walk comfortably and confidently once again.
Contact Information
Don’t wait until a minor foot issue becomes a major problem. Contact us today for specialized care tailored to your needs.
Toms River Office
📍 664 Commons Way Building 1
Toms River, NJ 08755
📞 Phone: (732) 557-9900
📧 Email: gsfagroup@gmail.com
Belleville Office
📍 1 Clara Maas Drive
Belleville, NJ 07109
📞 Phone: (973) 450-3035
🌐 Website: gsfagroup.com

0 Comments